
- NOTE:
Before you read from here, know that I am posting and saving this information for my own benefit; as well as for those of you that might want to know more about Casey's disease, diagnosis and prognosis. Or even for your own info.
.
.
.
Stolen from Handbook of Diseases, Copyright © 2003 Lippincott Williams & Wilkins
.
.
Good Morning,
Having done a million hours of searching online over the past 3 years, it has occurred to me that although I find interesting things about Chronic Pancreatitis, I have yet to find that 'magical' diagnosis/prognosis as it applies to her.
Casey has had two days of excruciating and debilitating pain. - Rough days for her...
.
.
.
.
Please pray.
*Please do not feel as though you must read this all.
XOXO
Me
*******.
Free Web Counter
.
.
.
 I hope that is large enough to read..
I hope that is large enough to read..
.
.
.
Copyright Details for bottom two pictures: Professional Guide to Diseases (Eighth Edition), Copyright © 2005 Lippincott Williams & Wilkins.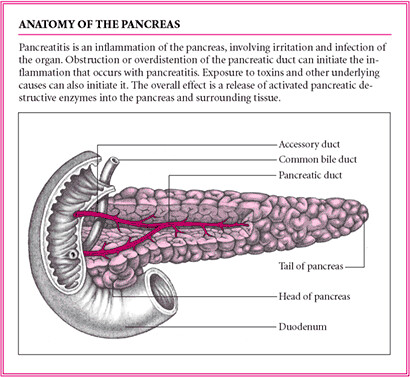
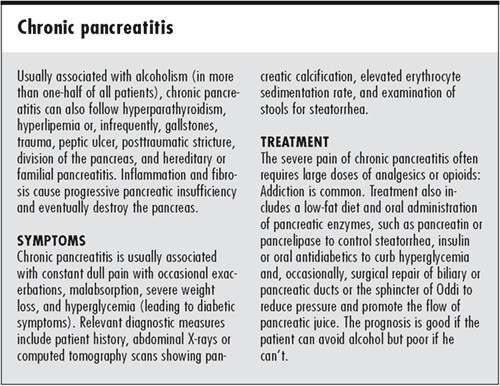
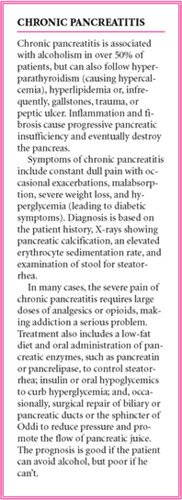
Chronic Pancreatitis:
- Chronic Pancreatitis is an ongoing inflammation of the pancreas over a prolonged period. Most cases of chronic pancreatitis are caused by alcohol overuse.
- Complications of Chronic Pancreatitis are secondary conditions, symptoms, or other disorders that are caused by Chronic Pancreatitis. In many cases the distinction between symptoms of Chronic Pancreatitis and complications of Chronic Pancreatitis is unclear or arbitrary.
- Chronic pancreatitis is a painful condition of the pancreas.
- Some evidence suggests that chronic pancreatitis may increase the risk of pancreatic cancer.
(Source: excerpt from What You Need To Know About Cancer of the Pancreas: NCI)
********
Treatment (Tx)
- I.V. fluid replacement,
- morphine,
- diazepam,
- antibiotics,
- calcium gluconate,
- insulin
********
The list of complications that have been mentioned in various sources for Chronic Pancreatitis includes:
- * Abdominal pain
- * Diabetes
- * Mild hyperglycemia
- * Malabsorption
- * Pancreas calcification
- * Insulin deficiency
- * Glucagon deficiency
- * Hypoglycemia unawareness
- * IGT (Impaired Glucose Tolerance)
- * Diabetes
- * Type 1 Diabetes
- * Type 2 Diabetes
- * Pancreas cyst
- * Pancreas abscess
********
Complications and sequelae of Chronic Pancreatitis from the Diseases Database include:
- * Diarrhea
- * Hyperglycemia
- * Back pain
- * Parotid gland enlargement
- * Pancreatic pseudocyst
- * Abdominal pain
- * Malabsorption syndrome
********
Obstruction
- Gallstone pancreatitis
- Choledocholithiasis
- Ampullary tumors
- Pancreatic tumors
- Metastatic carcinoma to pancreas
- Periampullary diverticulum
- Choledochocele
- Choledochal cyst
- Duodenal cyst
- Pancreatic calculi
- Pancreatic duct stricture*
- Pancreatic pseudocyst
- Pancreatic abscess
- Sclerosing cholangitis
- Hypertensive sphincter of Oddi
********
Congenital/inherited disorders
- Pancreas divisum*
- Hereditary pancreatitis*
- Cystic fibrosis*
- Annular pancreas
- Heterotopic pancreas
- Duodenal duplication
- Alpha1-antitrypsin deficiency*
********
Toxins
- Alcohol*
- Methanol
- Organophosphate insecticides
- Scorpion venom
- Occupational chemicals
********
Drugs
- Azathioprine
- 6-Mercaptopurine
- Thiacide diuretics
- Furosemide
- Ethacrynic acid
- Tetracycline
- Sulfonamides
- Nitrofurantoin
- Metronidazole
- Erythromycin
- Pentamidine
- Didanosine
- Sulfasalazine
- 5-Acetylsalicylic acid products
- l-Asparaginase
- Oral contraceptives
- Corticosteroids
- Estrogens
- Valproic acid
- Methyldopa
- Cimetidine
- Ranitidine
- Sulindac
- Acetaminophen
- Salicylates
- Octreotide
********
Metabolic disorders
- Hypertriglyceridemia
- Hypercalcemia
- Hyperparathyroidism*
********
Trauma
- Blunt or penetrating trauma*
- Surgical trauma
- Endoscopic retrograde cholangiopancreatography
- Endoscopic sphincterotomy
- Sphincter of Oddi manometry
********
Vascular causes
- Postoperative pancreatitis
- Atherosclerotic emboli
- Cardiopulmonary bypass surgery
- Malignant hypertension
- Ergotamine overdose
- Systemic lupus erythematosus
- Polyarteritis nodosa
********
Infections
- Bacterial Mycoplasma
- Campylobacter jejuni
- M. tuberculosis
- Legionella
- Leptospirosis
- M. avium complex
********
Viral
- Mumps
- Rubella
- Hepatitis A, B, C
- HIV
- CMV
- Coxsackievirus B
- Epstein-Barr
- Adenovirus
- Varicella
- Echo virus
Fungal:
Candida albicans infection
Aspergillosis
********
Parasitic
- Clonorchiasis
- Ascariasis
- Cryptosporidiosis
- Toxoplasmosis
********
Miscellaneous
- Penetrating gastrointestinal ulcer
- Duodenal Crohn's disease
- Protein-calorie malnutrition
- Tropical pancreatitis*
- Reye's syndrome
- Hypothermia
- Idiopathic pancreatitis*
- Posttransplantation
- Food allergy
- Chronic renal insufficiency
- Severe burns
- Long-distance running
- Bulimia
- Eosinophilic pancreatitis
********
- ❑ Acute and Chronic pancreatitis is a life-threatening emergency. Provide meticulous supportive care, and continuously monitor the patient.
- ❑ Monitor the patient vital signs and pulmonary artery pressure closely.
- ❑ Monitor the patient fluid intake and output and electrolyte levels.
- ❑ Assess the patient for crackles, rhon-chi, decreased breath sounds, or respiratory failure.
- ❑ Observe the patient for signs of calcium deficiency, such as tetany, carpopedal spasm, cramps, and seizures.
********
CLINICAL TIP:
Serum calcium levels decrease in acute pancreatitis, possibly from fat necrosis, resulting in a binding of calcium with free fatty acids.
- Muscle twitching,
- tremors,
- and irritability are signs of decreased calcium levels.
- ❑ Administer analgesics, as needed, to relieve the patient’s pain and anxiety.
- ❑ Observe the patient for adverse reactions to antibiotics: nephrotoxicity with aminoglycosides, pseudomembranous enterocolitis with clindamycin, and blood dyscrasias with chloramphenicol.
- ❑ Monitor the patient for complications due to total parenteral nutrition, such as sepsis, hypokalemia, overhydration, and metabolic acidosis.
- ❑ Observe the patient for signs of sepsis, such as fever, cardiac irregularities, changes in arterial blood gas measurements, and deep respirations.
********
National Digestive Diseases Information Clearinghouse
2 Information Way
Bethesda, MD 20892-3570
E-mail: nddic@info.niddk.nih.gov
The National Digestive Diseases Information Clearinghouse (NDDIC) is a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). NIDDK is part of the National Institutes of Health under the U.S. Department of Health and Human Services. Established in 1980, the clearinghouse provides information about digestive diseases to people with digestive disorders and to their families, health care professionals, and the public. NDDIC answers inquiries; develops, reviews, and distributes publications; and works closely with professional and patient organizations and Government agencies to coordinate resources about digestive diseases.
Publications produced by the clearinghouse are reviewed carefully for scientific accuracy, content, and readability.
This e-text is not copyrighted. The clearinghouse urges users of this e-pub to duplicate and distribute as many copies as desired.
********
Topic Author(s): Arnold C. Friedman, MD
Submitted by: Gastrointestinal Learning File -
© ACR -
Author Info Affiliation: ACR Learning File® Approved By: James G. Smirniotopoulos, M.D. -
Editor Info Affiliation: Uniformed Services University
********
In the Western Hemisphere, Europe, and Japan the most common cause of chronic calcifying pancreatitis is alcoholism. Other etiologies include idiopathic (up to 40%), biliary tract disease (usually acute rather than chronic), hyperparathyroidism, hereditary pancreatitis, cystic fibrosis, trauma, tropical pancreatitis, and hyperlipidemia.
********
CLINICAL FINDINGS:
Chronic pancreatitis can present with mild recurrent bouts of pain, constant abdominal or back pain, or in a small number of patients, painless exocrine and endocrine deficiency. Alcoholism is usually present for 5-10 years prior to the development of clinical pancreatitis. Initially, exocrine function is minimally impaired, but as insufficiency develops, fat and protein malabsorption occur with weight loss. Diabetes occurs in 10% of cases and impaired glucose tolerance in 14-90%. Duodenal obstruction and/or obstructive jaundice may occur in 45% of patients with moderate or advanced chronic pancreatitis.
********
PATHOLOGY:
Chronic calcifying pancreatitis is characterized by a nodular, misshapen, hard gland that can be enlarged or shrunken. Calculi are present and are almost always within the ductal system. They vary in size from microscopic concretions to 1-2 cm stones.
********
RADIOLOGY:
Demonstration of pancreatic lithiasis on plain films is a fast and inexpensive means of confirming a clinical diagnosis of chronic pancreatitis and effectively excluding carcinoma. In various series the frequency of plain film calcification has varied from 20 to 50% in alcoholic chronic pancreatitis. By contrast, only 2% or less of patients with chronic pancreatitis from biliary disease develop pancreatic calculi.
********
SONOGRAPHY:
Due to the presence of fibrosis within the gland, there is sometimes sonographic evidence of an inhomogeneously abnormal echo texture often accompanied by calcifications.
These calcifications are in the ductal system; their distribution may be focal or diffuse, and if large enough they are associated with acoustical shadowing. The gland is often irregular in outline and there may be enlargement (focal or diffuse) or parenchymal atrophy. Pancreatic ductal dilatation is often visible due to obstructing stones or stricture.
Chronic pancreatitis can be associated with thrombosis of the portal venous system. This usually involves the splenic vein; however, extension to involve the main portal vein can also occur.
Echogenic thrombus may be identified within the involved portion of the vein accompanied by demonstration of collateral channels. In some instances, the obstructed vein itself cannot be sonographically identified.
********
CT:
The gland in chronic pancreatitis can be normal in size or enlarged or it may be small, atrophic and replaced by fat. When the gland is enlarged, this enlargement may be focal or diffuse. Focal enlargement due to chronic pancreatitis (which is nearly always in the pancreatic head) is hard to distinguish on CT grounds alone from carcinoma unless punctate calcifications are present as these are almost never found in carcinoma (except sometimes following chemotherapy). The incidence of pancreatic carcinoma is low (except for familial pancreatitis) in patients with chronic pancreatitis. The calcifications that are often present in chronic pancreatitis are easily seen on CT (which is the most sensitive modality for their demonstration) and are usually multiple. They may occur in only one part of the gland or be present throughout.
Pancreatic ductal dilatation (greater than 3 mm) is often present, especially when a focal mass with calcification involves the head.
The ductal dilatation may be irregular (73%),
smooth (15%),
or beaded (12%).
Common bile duct dilatation may be associated. Occasionally in chronic pancreatitis, CT may show only a markedly dilated beaded pancreatic duct which can simulate a number of small intrapancreatic pseudocysts.
The presence of thrombosis in the portal system can be inferred when a vein fails to opacify normally following intravenous contrast injection and collateral channels are demonstrated.
Patients with chronic pancreatitis can have all the symptoms and signs of pancreatic carcinoma. If a noncalcified focal mass is found in the pancreas of such a patient, then pancreatic carcinoma has to be considered. The presence of the characteristic dense calcifications of chronic pancreatitis within a mass makes it unlikely that it represents a pancreatic cancer. If a diagnostic dilemma exists, then a percutaneous needle aspiration should be considered.
********
False Positives/Negatives
Chronic pancreatitis and pancreatic carcinoma share many CT features, and occasionally, differentiation may be impossible. Obliteration of the fat sleeve around the superior mesenteric artery has been described in both chronic pancreatitis and pancreatic carcinoma.
Pseudotumoral enlargement around focal pancreatitis with extensive fibrous tissue proliferation usually fails to enhance after the administration of contrast material. This characteristic makes the differential diagnosis of pancreatic carcinoma difficult.
So tell me, did you get this far?
http://www.emedicine.com/med/TOPIC1721.HTM
Pancreatic calcifications, often considered pathognomonic of chronic pancreatitis, are observed in approximately 30% of cases.
********
PROGNOSIS
* The prognostic factors associated with chronic pancreatitis are age at diagnosis, smoking, continued use of alcohol, and the presence of liver cirrhosis.
* The overall survival rate is 70% at 10 years and 45% at 20 years. In an international study, 559 deaths occurred among patients with chronic pancreatitis, compared to an expected number of 157, which creates a standard mortality ratio of 3.6 (confidence interval 3.3-3.9). Taking the opposite view, the 10-year mortality rate is 30%, and the 20-year mortality rate is 55%.
* The risk of developing pancreatic cancer is approximately 4% at 20 years.
Source: Office of Rare Diseases
********.
Chronic Pancreatitis is listed as a "rare disease" by the Office of Rare Diseases (ORD) of the National Institutes of Health (NIH).
This means that Chronic Pancreatitis, or a subtype of Chronic Pancreatitis, affects less than 200,000 people in the US population.
Source - National Institutes of Health (NIH)- http://www.emedicine.com/med/topic1721.htm
Background
Chronic pancreatitis is commonly defined as a continuing chronic inflammatory process of the pancreas, characterized by irreversible morphological changes. This chronic inflammation can lead to chronic abdominal pain and/or impairment of endocrine and exocrine function of the pancreas. Chronic pancreatitis usually is envisioned as an atrophic fibrotic gland with dilated ducts and calcifications. However, findings on conventional diagnostic studies may be normal in the early stages of chronic pancreatitis, as the inflammatory changes can be seen only by histologic examination.
By definition, chronic pancreatitis is a completely different process from acute pancreatitis. In acute pancreatitis, the patient presents with acute and severe abdominal pain, nausea, and vomiting. The pancreas is acutely inflamed (neutrophils and edema), and the serum levels of pancreatic enzymes (amylase and lipase) are elevated. Full recovery is observed in most patients with acute pancreatitis, whereas in chronic pancreatitis, the primary process is a chronic irreversible inflammation (monocyte and lymphocyte) that leads to fibrosis with calcification. The patient with chronic pancreatitis clinically presents with chronic abdominal pain and normal or mildly elevated pancreatic enzyme levels; when the pancreas lose its endocrine and exocrine function, the patient presents with diabetes mellitus and steatorrhea.
Causes of chronic pancreatitis
The main causes of chronic pancreatitis include the following:
Alcoholism: Changes appear to develop slowly and may develop after excessive alcohol consumption for 10 years or more. Alcoholism is associated with chronic pancreatitis in 70% of patients.2
Cholelithiasis: Cholelithiasis is a common cause of acute pancreatitis, but it probably is associated with chronic pancreatitis in 20-25% of patients.3
Idiopathic: Etiology is idiopathic in 20% of patients.2
Drug use: Usually, drug-induced pancreatitis is an acute process and does not evolve into a chronic form.
Hereditary causes: Hereditary pancreatitis is an autosomal dominant disorder. Symptoms usually appear in the patient's first decade of life and eventually lead to both exocrine and endocrine pancreatic dysfunction.
Autoimmune disease: Autoimmune pancreatitis is a rare condition that is often seen in patients with primary sclerosing cholangitis.
Congenital causes: A congenital abnormality of fusion, pancreas divisum, can cause chronic pancreatitis
Cystic fibrosis: This disease is associated with pancreatic atrophy and chronic pancreatitis
Other conditions: Hyperlipidemia, hyperparathyroidism, and uremia can cause chronic pancreatitis.
Categories of chronic pancreatitis
Chronic pancreatitis can be classified into 3 categories: (1) chronic calcifying pancreatitis, (2) chronic obstructive pancreatitis, and (3) chronic inflammatory pancreatitis.
Chronic calcifying pancreatitis
Chronic calcifying pancreatitis is invariably related to alcoholism. The earliest finding is precipitation of proteinaceous material in the pancreatic ducts that forms protein plugs that subsequently calcify. The ducts and lobules are initially involved in a random manner, and they are surrounded by normal parenchymal tissue. However, as the disease progresses, these normal areas become more diffuse. The pancreatic ductal epithelium undergoes atrophy, hyperplasia, and metaplasia at the site of the protein plugs. Many of the small pancreatic ductules dilate, while others are obliterated by fibrosis.
The main pancreatic duct shows a chain-of-lakes appearance due to alternating stenoses and dilatation. In approximately 50% of patients with chronic calcific pancreatitis, the pancreatic parenchyma contains cysts of varying sizes (several millimeters to 5 cm). These cysts are lined by cuboidal epithelium and contain pancreatic enzymes. Peripancreatic fibrosis is usually a late finding that involves the portal and/or splenic veins. Peripancreatic fibrosis causes stenosis or occlusion of retroperitoneal lymph channels. Ascites may complicate chronic calcific pancreatitis as a result of portal hypertension or lymphatic obstruction in 1-2% patients.
Chronic obstructive pancreatitis
In chronic obstructive pancreatitis, the prominent histologic changes are periductal fibrosis and subsequent ductal dilatation. These changes are much more focal than those in the other forms, and in most patients, the changes involve only the portion of the pancreas in which ductal drainage is impaired. Diffuse changes may occur, in which the main pancreatic duct or ampulla is obstructed. Although protein inspissation may occur, histologic changes in the ductal mucosa are less common, and calcification is unusual. Moreover, the pancreatic duct is dilated, and the pancreas is normal in size, atrophic, or focally and/or globally enlarged. A variety of factors are implicated in chronic obstructive pancreatitis; these include ductal obstruction due to ampullary stenosis, inflammatory or neoplastic causes, surgical ductal ligation, and fibrosis due to a pseudocyst as a complication of an episode of acute pancreatitis.
Chronic inflammatory pancreatitis
Chronic inflammatory pancreatitis is rare and can affect elderly persons without a previous history of alcohol excess.
Autoimmune pancreatitis
Autoimmune-related chronic pancreatitis is a distinct clinical entity, which may present with signs of acute or chronic pancreatitis, sometimes associated with cholestatic jaundice. On imaging, it may appear as diffuse (duct destructive) or pseudotumoral lesions. These 2 aspects are probably different clinical forms of chronic autoimmune pancreatitis.4
Some autoimmune diseases are associated with chronic autoimmune pancreatitis, but not consistently. One such disease involves a bile disorder that is very similar to primary sclerosing cholangitis but is responsive to corticosteroid treatment. Pancreatitis may be associated with Crohn disease and ulcerative colitis and thus provides justification to investigate patients with idiopathic pancreatitis for underlying inflammatory bowel disease. Chronic autoimmune pancreatitis must always be considered in patients with a pancreatic mass that is atypical for carcinoma on imaging or clinical findings. Corticosteroid therapy for 4 weeks in patients with pancreatic adenocarcinoma is probably less harmful than pancreatectomy (or chemotherapy) in patients with chronic autoimmune pancreatitis.
Diagnosis depends on clinical and radiologic findings. The diagnostic value of serologic markers and, especially, autoantibodies must still be clarified.
Non-alcoholic duct destructive chronic pancreatitis
http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1891454
******
http://www.emedicine.com/radio/topic522.htm
Degree of Confidence
Currently, CT is regarded as the imaging modality of choice for the initial evaluation of suggested chronic pancreatitis. The diagnostic features of pancreatic enlargement, pancreatic calcifications, pancreatic ductal dilatation, thickening of the peripancreatic fascia, and bile duct involvement are depicted well on CT scans.
CT is more sensitive than plain radiography and ultrasonography in the depiction of pancreatic calcification. Moreover, CT depicts calcification in the pancreas, and confusion with nonpancreatic calcification is less likely. The accuracy of CT is 59-95%; the wide variation is due to the wide discrepancy in the criteria used for diagnosis and in the quality of CT scanners. CT helps in the diagnosis of atrophy of the pancreas, providing better results than ultrasonography.
False Positives/Negatives
Chronic pancreatitis and pancreatic carcinoma share many CT features, and occasionally, differentiation may be impossible. Obliteration of the fat sleeve around the superior mesenteric artery has been described in both chronic pancreatitis and pancreatic carcinoma.
Pseudotumoral enlargement around focal pancreatitis with extensive fibrous tissue proliferation usually fails to enhance after the administration of contrast material. This characteristic makes the differential diagnosis of pancreatic carcinoma difficult.
Findings
In most patients, a normal pancreatic duct is seen on images obtained with T2-weighted short-tau inversion recovery MRI sequences and MRCP. MRCP may depict the characteristic beaded appearance of the pancreatic duct in chronic pancreatitis. Pancreatic duct calculi are depicted as round filling defects. In chronic pancreatitis, fat-suppressed T1-weighted images usually show a loss of signal intensity. This loss is explained by the fact that pancreatic fibrosis decreases the proteinaceous fluid content of the pancreas, resulting in loss of pancreatic signal intensity. Fibrosis is associated with decreased vascularity, which causes decreased pancreatic gadolinium enhancement.
Small punctate pancreatic calcification is difficult to detect by using MRI, but larger calcifications may be seen as foci of a signal void. As a result of its ability to depict fluid, T2-weighted MRI may demonstrate pancreatic and common bile duct irregularities and pseudocysts associated with chronic pancreatitis.
Parenchymal gadolinium enhancement is a useful technique in evaluating focal areas of inflammation. Compared with normal pancreatic segments, inflamed areas have decreased enhancement in the arterial phase and increased enhancement in the equilibrium phase.
Currently, the diagnosis of early chronic pancreatitis is difficult. With future improvement in spatial resolution and with the use of secretin-enhanced pancreatography, the detection of subtle changes of the side branches may allow the earlier noninvasive diagnosis of chronic pancreatitis. Secretin-enhanced pancreatography also has the potential to depict the anatomic relationships of pancreatic ducts and pseudocysts and to aid in the evaluation of pancreatic exocrine function.
Gadolinium-based contrast agents (gadopentetate dimeglumine [Magnevist], gadobenate dimeglumine [MultiHance], gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol [ProHance]) have recently been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). For more information, see the eMedicine topic Nephrogenic Fibrosing Dermopathy. The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. As of late December 2006, the FDA had received reports of 90 such cases. Worldwide, over 200 cases have been reported, according to the FDA. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with troublemoving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness. For more information, see the FDA Public Health Advisory or Medscape.
Degree of Confidence
Because of the introduction of faster imaging sequences and phased-array coils, the accuracy of MRCP has improved considerably, although some concern remains regarding the resolution of smaller pancreatic ducts.
Secretin-enhanced MRCP improves the detection of diseased pancreatic ducts when no abnormality can be shown in physiologic conditions. It also provides additional functional information regarding pancreatic exocrine function. As experience grows, MRI imaging, particularly MRCP, may be increasingly used in assessing and screening for chronic pancreatitis.
False Positives/Negatives
Standard good-quality protocols are important with MRCP; otherwise, poor examination technique may create false lesions, which may increase the frequency of unnecessary ERCP examinations.
---
http://www.scribd.com/doc/6072761/Metabolism-and-Elimination
---
---

Good morning Rock,
ReplyDeleteLots of good information there.. Sorta confusing and scary though.. I didnt see anything that shows something about repair and/or a solution for her. Very scary that!
JT brought up a point.. which Im sure you have considered but Im gonna share anyways..
Have you gone to WebMD or any other site that might give you a specialist on the pancreas... Then contact this specialist to see if he would at least look at her records to see if there was something in his knowledge he could or would share.
I realize money is an issue.. and his location might be a whole nother problem.
Anyways.. my love to all of you guys...
Mucho hugs
beepluvsrock.com
What a thing to have to live with. Poor Casey.
ReplyDeletesending a private note
ReplyDeleteI'm going to vent for a moment~so please forgive me...
ReplyDeleteI AM SO SICK OF HEARING ABOUT CASEY BEING SICK!! I want her better dammit and I want someone to find out what the hell is going on with her. I don't EVER want to see another picture of that poor girl in a hospital (unless she's giving birth :P) I want to see pictures of that bright, beautiful face throwing balls to Miss Milly and Punk~or pictures of her and Greg snuggled up on the couch with Sputnik and reading a book to Master Gabriel. I want to see goofy pictures of her at Thanksgiving eating an entire turkey leg, not trying to keep down a cup full of Jell-O because that damn pancreas of hers won't let her enjoy some of Mama's good ole comfort food. I want to see pictures of her passed out on a pile of books because she was up studying all night long for an exam~not passed out with IVs in her arms because they have to drug her in order for her to get a few precious hours of sleep. I want to see pictures of my happy-go-lucky CaseyFace and her friend Jenna riding around on tricycles. UGH~I am so frustrated and I CANNOT even begin to understand how you feel my sweet friend. I wish there was something that I could do. Every time I read that Casey is sick, in the hospital, in pain~I just want to know WHY?!? Why does she have to endure when so many are so damn reckless with their own lives? And yet, she always still has a smile on her face. I hope NO ONE ever underestimates the power of that young woman. Strength like hers needs to be bottled and marketed~everyone could use a dose or two of that.
OK, my venting session is now over :D
ReplyDeleteYeah.
Me too.
~
Leaving for the hospital now...
ReplyDeleteXOXO
me
PS for Beep
Yes, we have contacted more than a few outside doctors here too.
...and me too!!
ReplyDeleteI wish I could do more than just vent...
ReplyDeleteAMEN and I second THAT! ^^^^
ReplyDeleteAll the research I've been doing has told me the same things... But there is no real cure that I have found... There is also no real documentation for someone Casey's age having chronic pancreatitis... Parts of me wonder if it isn't something else making her pancreas act like it is... I so wish I could offer more than virtual hugs and thoughts and prayers (I do believe there is power in prayer though!)
Please know that I love you and Casey both and want her to get better yesterday!
Love Ya,
Stasha
Wow I don't think I could say it any better than thersjo. I wish there was something I could do. She is such a strong person. I wonder where she gets it from;) I am keeping you all in my prayers.
ReplyDeleteHow is Master Gabriel and Big Sam?
Lots of love to you all! XOXOXOXO
Hi.Prayers for you all. We also deal with chronic illness in our house hold. Our youngest son spend a great deal of time in and outof the hospital(as do his older sister and brother). We know that it not only affects the patient but the famly of that patient. Caregivers are special people..and need support so that they may continue to be strong for their loved one. Ya'll take care and we will say prayers for you all
ReplyDeleteDenise(Joyce's daughter inlaw)
I third that!!!..We're all so "sick" of seeing that sweetheart "sick"..much love to you my friend and endless prayers!!! xoxo
ReplyDelete
ReplyDeleteSee my comment on my PRIVATE POST...
XOXO
Me
http://en.wikipedia.org/wiki/Chronic_pancreatitis
ReplyDeletehttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1891454
http://www.touchgastroenterology.com/endoscopic-therapy-chronic-pancreatitis-a7848-1.html
http://www.angelfire.com/md/danil/nephrology.html
ReplyDeletehttp://people.virginia.edu/~wmd4n/pgdt/ch3s5.html
http://www.angelfire.com/sc2/lupiebeth/digestiveterm.html
Dr. Pfau:
http://local.yahoo.com/info-30970213-pfau-patrick-r-md-adult-gastroenterology-clinic-madison
And I still cannot find why the drs. are requesting a 24 hour urine collection...
??
http://www.emedicine.com/med/topic1721.htm
ReplyDeleteBackground
Chronic pancreatitis is commonly defined as a continuing chronic inflammatory process of the pancreas, characterized by irreversible morphological changes. This chronic inflammation can lead to chronic abdominal pain and/or impairment of endocrine and exocrine function of the pancreas. Chronic pancreatitis usually is envisioned as an atrophic fibrotic gland with dilated ducts and calcifications. However, findings on conventional diagnostic studies may be normal in the early stages of chronic pancreatitis, as the inflammatory changes can be seen only by histologic examination.
By definition, chronic pancreatitis is a completely different process from acute pancreatitis. In acute pancreatitis, the patient presents with acute and severe abdominal pain, nausea, and vomiting. The pancreas is acutely inflamed (neutrophils and edema), and the serum levels of pancreatic enzymes (amylase and lipase) are elevated. Full recovery is observed in most patients with acute pancreatitis, whereas in chronic pancreatitis, the primary process is a chronic irreversible inflammation (monocyte and lymphocyte) that leads to fibrosis with calcification. The patient with chronic pancreatitis clinically presents with chronic abdominal pain and normal or mildly elevated pancreatic enzyme levels; when the pancreas lose its endocrine and exocrine function, the patient presents with diabetes mellitus and steatorrhea.
Pathophysiology
Non-alcoholic duct destructive chronic pancreatitis
ReplyDeletehttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1891454
********************
ReplyDeletehttp://www.emedicine.com/radio/topic522.htm
Degree of Confidence
Currently, CT is regarded as the imaging modality of choice for the initial evaluation of suggested chronic pancreatitis. The diagnostic features of pancreatic enlargement, pancreatic calcifications, pancreatic ductal dilatation, thickening of the peripancreatic fascia, and bile duct involvement are depicted well on CT scans.
CT is more sensitive than plain radiography and ultrasonography in the depiction of pancreatic calcification. Moreover, CT depicts calcification in the pancreas, and confusion with nonpancreatic calcification is less likely. The accuracy of CT is 59-95%; the wide variation is due to the wide discrepancy in the criteria used for diagnosis and in the quality of CT scanners. CT helps in the diagnosis of atrophy of the pancreas, providing better results than ultrasonography.
False Positives/Negatives
Chronic pancreatitis and pancreatic carcinoma share many CT features, and occasionally, differentiation may be impossible. Obliteration of the fat sleeve around the superior mesenteric artery has been described in both chronic pancreatitis and pancreatic carcinoma.
Pseudotumoral enlargement around focal pancreatitis with extensive fibrous tissue proliferation usually fails to enhance after the administration of contrast material. This characteristic makes the differential diagnosis of pancreatic carcinoma difficult.
Findings
In most patients, a normal pancreatic duct is seen on images obtained with T2-weighted short-tau inversion recovery MRI sequences and MRCP. MRCP may depict the characteristic beaded appearance of the pancreatic duct in chronic pancreatitis. Pancreatic duct calculi are depicted as round filling defects. In chronic pancreatitis, fat-suppressed T1-weighted images usually show a loss of signal intensity. This loss is explained by the fact that pancreatic fibrosis decreases the proteinaceous fluid content of the pancreas, resulting in loss of pancreatic signal intensity. Fibrosis is associated with decreased vascularity, which causes decreased pancreatic gadolinium enhancement.
Small punctate pancreatic calcification is difficult to detect by using MRI, but larger calcifications may be seen as foci of a signal void. As a result of its ability to depict fluid, T2-weighted MRI may demonstrate pancreatic and common bile duct irregularities and pseudocysts associated with chronic pancreatitis.
Parenchymal gadolinium enhancement is a useful technique in evaluating focal areas of inflammation. Compared with normal pancreatic segments, inflamed areas have decreased enhancement in the arterial phase and increased enhancement in the equilibrium phase.
Currently, the diagnosis of early chronic pancreatitis is difficult. With future improvement in spatial resolution and with the use of secretin-enhanced pancreatography, the detection of subtle changes of the side branches may allow the earlier noninvasive diagnosis of chronic pancreatitis. Secretin-enhanced pancreatography also has the potential to depict the anatomic relationships of pancreatic ducts and pseudocysts and to aid in the evaluation of pancreatic exocrine function.
Gadolinium-based contrast agents (gadopentetate dimeglumine [Magnevist], gadobenate dimeglumine [MultiHance], gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol [ProHance]) have recently been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). For more information, see the eMedicine topic Nephrogenic Fibrosing Dermopathy. The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. As of late December 2006, the FDA had received reports of 90 such cases. Worldwide, over 200 cases have been reported, according to the FDA. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin;
http://www.scribd.com/doc/6072761/Metabolism-and-Elimination
ReplyDeleteMetabolism and Elimination - Upload a Document to Scribd
ReplyDeleteMy Prayers are with all of you. I just got out of the hospital after being there for 4 months. I have Chronic Pancreatitis and I had pseudo cysts that were surgically removed with insertion of a Jejunum feeding tube. I finally came home with the feeding tube and still having problems. I am researching daily to see what else can be done. I have another appt with another specialist next week. I did find out that they are removing the pancreas in Chicago and replacing Immune system so that you are not so brittle. I got my pancreatitis from High triglycerides. I wish you all the best and if I can be of any help let me know. Until then I will continue to pray for all of you and add you to our prayer chain. God is the only hope we have and as upset and doubtful as we get we always have him in the end.
ReplyDeleteGod Bless
Emily R.
Stolen from Pancreatitis group:
ReplyDeleteArticle from THE PHILIPPINE STAR: The reported cause of actor Rico Yan's(Filipino celebrity)death is nightmare or bangungot. Medical investigators in China , Japan and several Asian countries who performed autopsies on persons who died from 'acute hemorrhagic pancreatitis' found out that the majority of them had eaten NOODLES as their supper. This was a startling finding. However, it wasn't the noodles that caused nightmares but DEHYDRATION. Imbibing even with a few drinks of alcohol or just eating noodles immediately before bedtime compound this on an empty stomach will trigger an electrolyte imbalance and other factors that causes a person to dehydrate or lose water. It is therefore advisable for a person to take several glasses of water before bedtime if he had a few or several alcoholic drinks. Avoid eating noodles before bedtime, but if you can not avoid it, allow at least two hours for the body to digest the noodles before hitting the sack and drink plenty of water. The most important thing is, never go thirsty when going to bed and be sure you have plenty of water during your 8-hour rest. http://wiki. answers.com/ Q/What_is_ the_cause_ of_acute_ hemorrhagic_ pancreatitis& src=ansTT
acute hemorrhagic pancreatitis a condition due to autolysis of pancreatic tissue caused by escape of enzymes into the substance, resulting in hemorrhage into the parenchyma and surrounding tissues.
Dorland's Medical Dictionary for Health Consumers. © 2007 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
------------ --------- --------- --------- --------- --------- -
acute hemorrhagic pancreatitis
n.
Acute inflammation of the pancreas accompanied by the formation of necrotic areas on the surface of the pancreas and in the omentum and, frequently, also accompanied by hemorrhages into the substance of the gland.
The American Heritage® Medical Dictionary Copyright © 2007, 2004 by Houghton Mifflin Company. Published by Houghton Mifflin Company. All rights reserved.
------------ --------- --------- --------- --------- --------- -
acute hemorrhagic pancreatitis
Etymology: Gk, haima, blood, rhegnynei, to gush, pan, all, kreas, flesh
a potentially fatal inflammation of the pancreas characterized by bleeding, necrosis, and paralysis of the digestive tract.
Mosby's Medical Dictionary, 8th edition. © 2009, Elsevier.
------------ --------- --------- --------- --------- --------- -
pancreatitis
inflammation of the pancreas.
------------ --------- --------- --------- --------- --------- -
acute hemorrhagic pancreatitis
a condition due to autolysis of pancreatic tissue caused by escape of enzymes into the substance, resulting in hemorrhage into the parenchyma and surrounding tissues. Seen most commonly in dogs, rarely in horses and pigs. Clinical signs include abdominal pain that may be severe and associated with cardiovascular shock, vomiting and diarrhea. Fatalities are not uncommon. In the longer term, the process may be slowly progressive, appearing clinically to be relapsing, often with eventual destruction of the islets of Langerhans that leads to diabetes mellitus. Called also acute pancreatic necrosis.
chronic pancreatitis
relapsing or continuing acute pancreatic necrosis. Called also relapsing pancreatitis.
focal pancreatitis
focal lesions discovered incidentally in patients dying of other disease, e.g. canine distemper, foot and mouth disease.
interstitial pancreatitis
inflammation of the interstitial tissue; may be acute or chronic.
necrotizing pancreatitis
see acute hemorrhagic pancreatitis (above).
relapsing pancreatitis
see chronic pancreatitis
http://medical- dictionary. thefreedictionar y.com/acute+ hemorrhagic+ pancreatitis
acute pancreatitis (acute hemorrhagic pancreatitis)
Description:
sudden, rather diffuse destruction of pancreas
Organs Involved:
pancreas
Who Is Most Affected:
middle life, men with 10-yr alcohol history
Etiology:
Causes:
70-90+% in US due t
Caseys reply...
ReplyDeletehttp://www.medicalnewstoday.com/youropinions.php?opinionid=30423
Excellent photos!
ReplyDeleteExcellent photos!
ReplyDeleteJust adding one more...
ReplyDelete-----------------
European Pancreas Center
http://www.klinikum.uni-heidelberg.de/Home.104340.0.html?&FS=0&L=en
What is the Pancreas?
The pancreas is a yellowish gland, ca. 15 cm long, 5 cm wide and 2-3 cm in diameter that lies horizontally across the upper part of the abdomen.
It can be roughly divided into three parts: the head, the body and the tail.
The pancreas head lies to the right side of the midline in close contact with the first part of the small intestine, known as the duodenum.
The pancreas tail extends to the left up to the spleen.
The body of the pancreas is located in front of the junction of a number of important blood vessels leaving the aorta (the main blood vessel carrying oxygenated blood from the heart). They supply blood to the liver, the stomach, the upper part of the intestine and the pancreas itself.
What are the causes of chronic pancreatitis?
In the west, excessive alcohol consumption is the common cause (80%) of chronic pancreatitis. However, not all cases are due to chronic over-consumption. Patients have varying degrees of alcohol tolerance, and in some cases the disease is triggered when consuming relatively small amounts.
Besides alcohol, there are other important causes for the disease. These include a tendency to chronic gallstones, genetic defects, certain conditions in the pancreatic ducts (pancreas divisum), medication and disorders of the metabolism.
Sometimes, no particular cause can be found.
What are the most frequently encountered symptoms of chronic pancreatitis?
* Pain
* Bloating
* Diarrhea
* Weight loss
* Symptoms related to the development of Diabetes mellitus
The Treatment of Chronic Pancreatitis
Treatment is determined by the patient's symptoms. Often, patients suffer from almost unbearable pain in the upper abdomen which can be either continuous or episodic Alcohol consumption must be discontinued as a first measure.
Pancreatic enzyme supplements can then be taken, alleviating the condition by suppressing pancreatic secretions (thus relieving the pressure on the pancreas) and restoring the digestive process. If this does not alleviate pain, medication should be the next option. Failing this, surgery must be considered.
Fatty deposits in the stool and/or diarrhoea are proof that the pancreas is not producing sufficient digestive enzymes. These must be substituted with a regular intake of an appropriate medication. The presence of the condition may also be verified by a pancreatic enzyme (elastase) found in the patient's stool.Fat content of the meal will determine how many capsules containing enzymes need to be taken. To ensure that these have the desired effect it is often necessary to curb the stomach's natural acid production with acid-blocking medication. It is also vital to ensure that the patient takes a sufficient amount of fat-soluble vitamins (A, D, E K). In some severe cases, these may have to be injected. A blood test will show whether this is necessary.
A rising blood sugar level is proof that not enough insulin is produced in the pancreas. Dietary measures alleviate this condition in a few cases only. Patients routinely need to take additonal doses of insulin to regulate blood sugar levels.
When is an operation required?
50% of patients with chronic pancreatitis will require surgery at some point.
As the procedures are very complicated, pancreatic surgery will usually be performed in specialised clinics.
Several reasons demonstrate why surgery is necessary:
1. Pain management is unsuccessful, even when using the most potent medication.
2. A chronically inflamed pancreas affects surrounding organs such as the duodenum (constraint or blockage), the bile duct, the main pancreatic duct and blood vessels behind the pancreas.
3. Suspicion that the condition masks pancreatic cancer.
Pseudo-cysts (cavities filled with fluids, caused by inflammation) are sometimes found. F
Casey you don't deserve this dear :( this is very sad indeed and we think our day is bad perhaps we all should look inwards and think of people like yourself. I know and can see you have a God given gift in you Mother, you are an outstanding person Anna really exceptional and Casey you are truly extraordinary, the both of you are out of the ordinary in many ways.
ReplyDeletehttp://ehealthforum.com/health/food-related-to-acute-pancreatitis-t144731.html
ReplyDeleteI am dealing with the samething. I have pancrea divisum that brings on the pancreatitis. I deal with the pain, but sure would like to find another solution that ERCP. Have anyone ever heard of successful replacement of the duct?
ReplyDeleteI am sorry for your pain Mr. Terence;
ReplyDeleteI did not miss your comment; nor did I anticipate that it might take so long for me to reply to you. My apologies for that. I am dealing with a few health matters of my own, (and that all had to take precedence over "thinking"). :-)
I do not know how old you are, or how long since your diagnosis, how you were diagnosed, or how you have been treated to date.
That said, I will still be of help to you.
There are 3 places that will be extremely helpful to you.
I sincerely hope you will join them, share your own story, join in the conversations, and replies to the blogs.
(The people really are helpful, kind, compassionate; and you may find more than a few that also have pancreatic~divisum).
2 of these sites are:
http://health.groups.yahoo.com/group/pancreatitis/
-AND-
http://www.top5plus5.com/Index.html
Way back when, when Casey's pain became so unbearable that she finally sought medical advice, she was hospitalized immediately due to her enzyme levels being off the charts.
Of course before that blood test, we thought that hers was just another episode of "a virus", the "flu", "food poisoning", (or whatever flavor of the day the ER docs had previously provided to us).
Anyway, at that point, she was then sent down to Froedtert in Milwaukee for to verify that she had divisum. The hospital in Green Bay had seen on her CT Scans that this was a definite possibilty.
If you have read any further on her story of her own disease, you have already learned that she didn't have divisum.
Shortly after the 6th visit to Milwaukee, she was dx'ed with Chronic pancreatitis.
We then erroneously thought that Mayo (Rochester) would help. They didn't, and unless you wish to be dismissed as Casey was, you will not go there. Casey had awful experiences there.
I will NEVER refer anyone to Mayo...
To save you much time and effort in trying to find answers, I beg you to contact Dr. Sutherland in Minneapolis.
He is one of the foremost doctors that deal with pancreas issues, deformities, etc. Plus, any and ALL matters of the digestive system... Perhaps even your duct replacement!
*** The Yahoo pancreatitis Group was where I finally was referred to Dr. Sutherland.
(Casey and I are eternally grateful to this group for their high praise for, and recommendation of Dr. Sutherland).
Should travel be an issue, I believe there are groups that would assist you to be able to get there to see him, although I do not know of any offhand.
Dr Sutherland's contact information is through his assistant, "Ann Marie".
She is a wonderful person; and very, very, helpful. I had written to her with Casey's medical history. Ann Marie not only replied but called us both within half an hour!
We were, (and remain), very impressed.
Ann Marie Papas, Administration
University of Minnesota
Transplantation Division
Department of Surgery
612-625-5609 Tel
612-624-7168 Fax
papas001@tc.umn.edu
Please, at the very least, contact Ann Marie with your story via email.
Again, that address is:
papas001@tc.umn.edu
For Dr. Sutherland's "Curriculum Vitae" please go to:
http://www.diabetes.umn.edu/prod/groups/med/@pub/@med/documents/asset/med_84287.doc
He has a 46-page history that will show you his impressive resume, and capabilities.
*** What it won't show you is his kindness or personality. After all the GI's "specialists" Casey had dealt with before finding him, we had expected him to be no different. (We were hugely wrong, thank God).
I WOULD REFER ANYONE TO HIM!
flintville wrote today at 2:39 PM
ReplyDeleteI found this through the Wolters Kluwer website for you and cross~referenced it, finding the article linked below.
http://journals.lww.com/pancreasjournal/pages/default.aspx
XOXO
Me
http://en.wikipedia.org/wiki/Hemosuccus_pancreaticus
"The causes of hemosuccus pancreaticus can be grouped into diseases of the pancreas and diseases of the vascular structures around the pancreas. Diseases of the pancreas include acute and chronic pancreatitis,[8] pancreatic cancer,[2] pancreatic duct stones,[9] ruptured aneurysms of the splenic artery,[3] and pseudoaneurysms of the splenic artery[10] and hepatic artery.[11] Pseudoaneurysms are complications of pancreatitis where a pseudocyst is formed, with one wall abutting an artery, usually the splenic artery. Should the arterial wall rupture, the pseudoaneurysm will hemorrhage into the pancreatic duct.
Rarely the bleeding is not channeled into the bowel from the main pancreatic duct (or duct of Wirsung), but rather comes from the accessory pancreatic duct (or duct of Santorini). The former is termed Wirsungorrhage and the latter is termed Santorinirrhage. Bleeding from the duct of Santorini can be caused by pancreas divisum, a possible congenital cause of pancreatitis.[12]. "
All links are clickable at the bottom of the wiki page. Interesting info to discuss with your doctor.
XOXO
Me
Pancreatitis caused by statins first started appearing in the medical literature as early as 1990. All statins currently in use reportedly can cause pancreatitis, a not surprising observation when one considers that all statins are reductase inhibitors and can be expected to have similar side effect profiles. Both chronic and acute pancreatitis are curable. Fasting is often needed for a few days or sometimes even weeks to heal the pancreas. Intravenous (IV) fluids are used to maintain nutrition while fasting. Sometimes a surgery to drain the abdomen is needed. People with chronic pancreatitis often take pills with enzymes to help them digest their food. The change of daily living habits is also necessary to avoid immediate danger. Pancreatitis can be either acute or chronic. Pancreatitis' most common cause is high alcohol intake. It has many unpleasant symptoms, and it can be cured in multiple ways. Acute and chronic pancreatitis have similar symptoms.
ReplyDeleteWant some bigger muscle under the guidance of expert Trainer, find it here at visual impact muscle building review
Pancreatitis kills.
ReplyDeleteAnd NO. Pancreatitis canNOT be cured.
Nor is the most common cause alcohol.
Learn your facts before you comment.
Thank you
Pancreatitis kills.
ReplyDeleteAnd NO. Pancreatitis canNOT be cured.
Nor is the most common cause alcohol.
Learn your facts before you comment.
Thank you
http://www.diabetes.co.uk/news/2012/Mar/artificial-pancreas-breakthrough-for-diabetes-treatment-96492172.html
ReplyDeleteArtificial pancreas breakthrough for diabetes treatment
Tue, 06 Mar 2012
One of the many companies working on a commercially available artificial pancreas has developed a prototype of a fully synthetic artificial glucose sensing system, a key part of its glucose-sensing microchip for treating patients with type 1 diabetes.
The system, described as a mission-critical component by PositiveID, is an integral part of an artificial pancreas and can sense and respond to levels of glucose in human plasma. Until now, it had only been shown in a model blood plasma matrix. An artificial pancreas should be able to offer both a continuous glucose monitor and an insulin pump to bring automatic checks on blood sugar levels in the body for people suffering from diabetes.
William Caragol, chairman and chief executive of the company, commented "The development of a fully implantable glucose sensor is one of the essential requirements for the successful development of an artificial pancreas."
He added "We are well positioned to play a potentially significant role in making an artificial pancreas a reality for people with type 1 diabetes."
The news comes after another United States company recently announced clinical trial findings that showed it was getting nearer to realising an insulin delivery system that achieved clinical endpoints with low-glucose suspend technology.
ReplyDeleteI have also found an awesome site if you wish to see radiographical images of your pancreas- http://www.radiologyassistant.nl/en/47a07dcd6498c
Also for Casey:Re: Endometriosis http://www.radiologyassistant.nl/en/4da490c32edcc
Pancreas: (Acute) Pancreatitis
Diagnosis and InterventionThomas Bollen, Marieke Hazewinkel and Robin SmithuisRadiology department of the St. Antonius hospital, Nieuwegein, the Medical Centre Alkmaar and the Rijnland hospital, Leiderdorp, the NetherlandsIntroductionImaging of Acute PancreatitisClassification of Acute PancreatitisCT Severity IndexInterstitial pancreatitisExudative Panc